Refusal and reluctance of some states to expand Medicaid presents obstacle to coverage expansion
 The Patient Protection and Affordable Care Act mostly stands and, with it, the prospect that 30-some million more Americans will get health insurance. What the U.S. Supreme Court decided on strictly legal grounds, Catholic health leaders welcomed as a matter of basic social justice, consistent with the church's view of health care as a universal human right and with the Catholic health ministry's mission to care for all, including society's most at-risk and marginalized.
The Patient Protection and Affordable Care Act mostly stands and, with it, the prospect that 30-some million more Americans will get health insurance. What the U.S. Supreme Court decided on strictly legal grounds, Catholic health leaders welcomed as a matter of basic social justice, consistent with the church's view of health care as a universal human right and with the Catholic health ministry's mission to care for all, including society's most at-risk and marginalized.
The gratified reaction of Robert J. Henkel, president and chief executive of St. Louis-based Ascension Health, the nation's largest nonprofit Catholic system, was typical. "Our goal and objective is having 100 percent insured and 100 percent access to health care for everyone in this country," he said. The law "doesn't get us all the way there" but it's "a great leap in that direction."
Joseph R. Swedish, president and chief executive of Trinity Health of Novi, Mich., and chair of the CHA board, said, "Catholic health care providers are generally pleased with the Supreme Court's ruling, but we knew, upon passage, that the ACA was not perfect. It will still require many modifications as we move forward, and I'm certain we will be actively engaged in those discussions, just as we have been in the past."
The court's much anticipated June 28 ruling ended more than two years of legal uncertainty over the ACA. "There is a general feeling that now that we know what's in and what's out, we can make decisions faster," said Deb Fischer-Clemens, vice president of the Avera Center for Public Policy, a unit of Sioux Falls, S.D.-based Avera Health. "... It makes it easier for us to look forward."
Swedish said: "The ruling gave us clarity regarding the constitutionality of the individual insurance requirement and allows us to move forward executing strategic initiatives that will help us create a meaningful and effective transformation of the nation's health care system. It's really too early to judge how effective the mandate will be because so much of its success depends on the state-by-state implementation of health insurance exchanges and adoption of the Medicaid expansion."
Medicaid expansion
Relief at the Supreme Court's decision to uphold the accountable care act requirement that most Americans buy health insurance was tempered by the justices' equally surprising ruling on the law's feature extending the federal-state Medicaid program to people under age 65 with incomes up to 133 percent of the poverty level. By striking down a provision that would have penalized noncompliant states with the potential loss of all of their existing federal Medicaid funds, the Supreme Court effectively freed states to opt out of the expansion, which had been projected to account for roughly half of the law's new insured people.
Michael Slubowski, president and chief executive of the Denver-based Sisters of Charity of Leavenworth Health System, predicted that, despite their current grumblings and protests, the reticent states will eventually fall into line, persuaded by the law's promise that the federal government will pay 100 percent of states' new ACA-related Medicaid expenses until 2017 and no less than 90 percent afterwards. Besides, he added, there will be "a lot of political opposition from consumers and the general public" in states that refuse to go along with the expansion of Medicaid.
State participation
Just as state participation is central to the law's goal of insuring 17 million low-income individuals and families through expansion of Medicaid, it is key to providing access to meaningful and affordable private health insurance to small businesses and individuals. The law requires the creation of state-based exchanges through which individuals and small businesses can buy credible, affordable coverage. Beginning in 2014, individuals of modest to moderate means with incomes from 100 percent to 400 percent of poverty will be eligible for premium and cost-sharing subsidies for insurance purchased through an insurance exchange.
Chris Lee, a communications officer for the nonpartisan Kaiser Family Foundation, said that in states that decline to comply with the ACA's Medicaid expansion, and where current programs do not cover all individuals with incomes at or below the poverty line — $11,170 for an individual, or $23,050 for a family of four — some very low-income individuals may be excluded from Medicaid and be ineligible for subsidies in the exchanges. Health and Human Services Secretary Kathleen Sebelius has written that the law provides financial hardship exemptions from the mandate for individuals, and HHS will establish, as needed, additional hardship exemptions for people who live in states that do not expand their Medicaid programs in line with the ACA.
Medicaid expansion could be unlikely in three of the four states served by St. Louis-based SSM Health Care. The implications of decisions by Wisconsin, Oklahoma or Missouri not to expand Medicaid would be "that some of the most economically vulnerable will not be covered and will still rely on the emergency room for their care," said Dixie Platt, SSM senior vice president of communications, public policy and external relations. "If people had access to health care services sooner, they would avoid the emergency room, get the care they need before an illness becomes dire and reduce overall health care cost," she said.
Insurance exchanges
The Congressional Budget Office estimates that 20 million people — including a significant number of individuals who had prior coverage — will be covered by policies purchased through the exchanges.
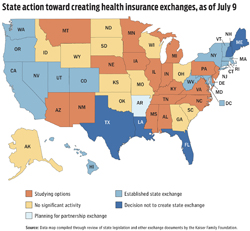
Building an exchange is a layered undertaking requiring states to find political consensus, set out essential health benefits, establish carrier requirements, set up financing structures and build sophisticated information technology systems. According to the Kaiser Family Foundation, as of July 2, 15 states had established exchanges, one was planning a partnership exchange, eight were studying options, 12 had not undertaken any significant activity and five had announced they would not create a state exchange.
States that do want to meet ACA deadlines to launch state-run exchanges will have to move on an aggressive timeline, according to Kaiser. HHS will begin certifying "exchange readiness" in November and exchanges must be fully operational by the law's launch deadline of Jan. 1, 2014. States that do not meet the deadline or decline to set up exchanges will default to a federal exchange or a federal-state partnership model.
State variance adds to complexity
Multistate systems are especially attuned to the speeds and extents to which the states comply with the letter and spirit of the law. The states' varying responses add up to "another level of complexity" for Catholic Health Initiatives, based in Englewood, Colo., and with facilities in 19 states, said M. Colleen Scanlon, the system's senior vice president of advocacy. Trinity's Swedish added, "Being in 10 states, we're trying to be prepared" — and prepared as well for "lingering problems" inherent in the act itself and subject to regulations and clarifications yet to come.
Alan Yordy, president and chief mission officer of PeaceHealth of Vancouver, Wash., also foresees challenges ahead. "I suspect, because there are so many moving parts in the law, we're going to have as many unintended consequences as things that work out well," he said.
This much, at least, is certain: The ACA is intended to increase health care value by improving care quality, lowering the rate of health care inflation and keeping people healthier by promoting prevention and better management of chronic disease. These goals are achievable, said Slubowski, by "moving the care into the community and the home."
Ascension Health's Henkel described the twin goals of lowering costs and increasing quality as going hand-in-hand: The better the care, the shorter the hospital stay, the fewer the complications and the lower the cost. And Ascension Health's own experience with quality improvement initiatives has proved it, he said.
Expanding access
Health executives said they have more than enough technical and inpatient capacity to accommodate the anticipated wave of newly insured. "We've been caring for these patients anyhow," said Sr. Laura Jean Wolf, OSF, president of Franciscan Sisters of Christian Charities Sponsored Ministries of Manitowoc, Wis. "What we hope will be different is that there will be reliable payments coming in." Even so, because many of those payments will cover less than full costs, bottom lines will remain under pressure. The Sisters of Charity of Leavenworth's Slubowski said of health reform: "We don't view this as a boon financially."
Scanlon said that just how many people in the ACA's target population will eventually make it onto the insurance rolls is now an open question. "Slippage," as she called it, could result not just from states dragging their feet on Medicaid expansion but also from individuals resisting the law's insurance requirement. Noting that the tax liability for people who decline to buy health insurance is considerably less than the cost of purchasing insurance, PeaceHealth's Yordy predicted many people will pay the tax rather than buy coverage. "We'll see if 30-32 million more get insurance," he said. "My view is we'll get half to two-thirds of the way there."
However many more people the law succeeds in covering, providers will have their work cut out because, as Henkel said, "Just providing insurance doesn't guarantee access." There's widespread agreement that the nation's health care system already lacks enough primary care capacity and that the expansion of coverage promised by the ACA will only widen the gap. CHI's Scanlon said, "We will try, along with everybody else, to expand the primary care (provider) population" to include not just more physicians but also advanced-practice nurses and physician assistants. Trinity Health's Swedish concurred, saying it will also be necessary to create new "access points" — primary care clinics, for example.
As Avera's Fischer-Clemens noted, the ACA's passage highlighted "a huge partisan divide." And it persists. The law's opponents in Congress are staunch in their vows to repeal it.
Slubowski expects the law to remain intact. "From my perspective, the cow is out of the barn, the genie is out of the bottle," he said. FSCC's Sr. Wolf also thinks the law will withstand political challenges. Her far greater concern, she said, is that the money to fund it won't be forthcoming.
Yordy said, no matter what, "Our mission really hasn't changed, ACA or no ACA. … We have a commitment to serve everyone who comes through our doors."
Even if the ACA delivers completely up to its promise, about 20 million people will still be uninsured — "left outside" the health care system, as Henkel put it, and he pledged Ascension Health will continue to advocate for them. Included in this marginalized group are millions of undocumented immigrants who are ineligible to participate in the Medicaid expansion or in the health exchanges. In his chairman's address at the 2012 Catholic Health Assembly, Swedish expressed certainty that "Catholic health care will continue to fill the void and serve this vulnerable and often marginalized group."