By JUDITH VANDEWATER
ATLANTA — Health care reform legislation being rolled out over the next few years envisions a health care system that is seamless and efficient for patients — one in which hospitals, physicians and other service providers work together to improve care, enhance population health and slow spending.
While such high-value, patient-centered care is a worthy goal, it won't be simple to achieve. Getting there will be a multistep process and one that may well prove the health care management equivalent of landing a man on the moon.
At a Catholic Health Assembly focused on the opportunities created by health reform, two senior ministry executives offered tips for deconstructing the challenge into actionable parts. The session reunited Michael A. Slubowski with his former colleague Michael Murphy. Slubowski is president and chief executive of the Sisters of Charity of Leavenworth Health System of Lenexa, Kan. Before he took the top spot at the Sisters of Charity in November, he was president of health networks for Trinity Health of Novi, Mich. Murphy is Trinity Health's executive vice president of health networks.
The speakers focused on ways to more closely align hospitals and ambulatory service providers with the practices of physicians. Such alignment, Slubowski said, is the foundation for success in the emerging health care economy.
 Challenging transitions
Challenging transitions
Health reform promises to expand insurance coverage to nearly 92 percent of Americans. That is a huge achievement and one consistent with the ministry's mission and core values, Slubowski said, but that advance comes with a clear operating challenge for hospitals and health systems. "We will have to care for more people at a lower total cost per capita. At the end of the day, we are going to have to achieve improvement just to stay even."
As part of health reform, health leaders must manage a transition from fee-for-service medicine with a bias toward physician specialists to a system that will pay for performance and put a greater focus on primary care. Thriving in the new environment will require a high degree of integration between physicians and health systems to improve care management, Slubowski said.
"First and foremost, the important thing in physician alignment is to remember the goal is clinical integration," he said. "At the end of the day, if we can't develop a system in which we share responsibility for care coordination and outcomes for patients that we serve, I think we've lost our way."
Service integration
The health reform law gives incentives for accountable care organizations to hold physicians, hospitals and ambulatory care and other providers jointly responsible for managing the health needs of groups of Medicare recipients. But Medicare will not be the only payer expecting highly coordinated, efficient, clinically rigorous care from providers across care platforms. All payers are moving in that direction, the speakers said.
Murphy said that since no organization can afford to own facilities and provide service along the entire care continuum in all of the markets where it does business, it will be essential to build relationships among providers with the ultimate goal of aligning services and the financial interests of providers.
Gearing up
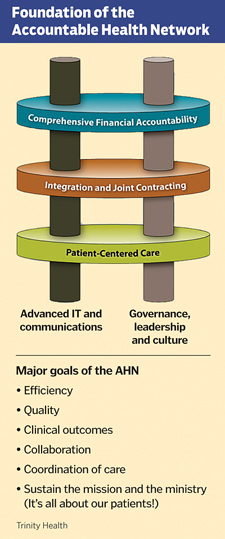
Trinity has identified five core sets of capabilities necessary for successful partnerships like these. They are: a requirement that all partners have access to advanced information technology to track patient care; compatible governance, leadership and cultures; a shared focus on patient-centered care; integration of services and joint contracting capability; and comprehensive financial accountability.
Murphy said Trinity assessed its readiness to participate in accountable care organizations on a market-by-market basis and developed three-year action plans in each market. It found that six of its markets were in the best position to develop accountable care organizations, three were making progress and six were less advanced in their ability to participate in pay-for-performance or financial risk-bearing contracts. "Accountable care is a journey," one that could take years to navigate, Murphy said.
Slubowski said a health system or hospital's alignment with physicians will be essential to reduce such cost drivers as high-end imaging, avoidable emergency department use and preventable Medicare readmissions within 30 days of hospital discharge.
Purchase frenzy
He referenced the "new frenzy" by hospitals to employ physicians and purchase physician practices. Competition is bidding up the purchase prices to the point at which many practices will never be able to generate a return on investment, he said, adding that decisions being made today will have long-term repercussions for the practice of medicine.
Citing The New England Journal of Medicine, Slubowski said more than half of the practicing physicians in the U.S. are now employed by hospitals or integrated practice groups. In addition to employed physicians, hospitals contract for physician services and have relationships with community physicians.
To improve physician alignment, hospitals are attempting to get private practice doctors to agree to follow at least some evidence-based clinical care protocols. They are offering management and IT support to improve performance and practice. With employed and contracted physicians, hospitals are attempting to move to more performance-based cultures.
Slubowski said it will be critical to develop physician and administrative leaders to lead delivery transformation and physician alignment efforts. "We are going to have to have physician and administrative leaders that are equipped to manage the physician network well and to really create a group practice culture. We are going to need folks who really can lead across the continuum of services whether it is home care or long-term care, senior services and the integration of the service. Then we need folks that can do work on accountable health networks, or OWAs," Slubowski's acronym for the "other weird arrangements" he expects to see during the transition to the delivery system of the future.
The ultimate goal of health reform and of clinical care integration is to improve care outcomes for patients, he said. For Catholic health providers, successfully navigating the change will provide the opportunity to advance the ministry. This will benefit patients and communities, improve care quality and provide more access to care, he said.