BARTHOLOMEW RODRIGUES, MDiv, MBA, BCC, WILLIAM VAUGHAN, MA, BCC, and JESSICA MOORE
Catholic Health
It has long been recognized that emotional and spiritual care plays an important role in one's well-being. Professionals in spiritual care and chaplaincy services who work in health care settings receive academic preparations and clinical training for this specialized healing ministry. They are a vital part of the health care team who contribute to a patient's overall health and wellness.
Nevertheless, the persistent stereotype of a hospital chaplain is someone who sits, listens and offers some philosophical platitudes to help ease the distress of a patient or client. However, there is more to it than simply "being present." Evidence-based ministry requires demonstrating how chaplaincy encounters help in the healing and recovery process and why these services must be established, maintained and integrated into the total interdisciplinary health care continuum. Spiritual care and chaplaincy should be an important part of the clinical documentation process.
To further advance an evidence-based approach to health care ministry for spiritual care and chaplaincy services, electronic medical records (EMR) can be a helpful tool to document encounters, interventions and outcomes. Done right, an EMR can harness the power of evidence-based health care chaplaincy through spiritual care assessments (including interventions and outcomes) and dashboards. Moreover, EMRs can serve as a platform to optimize resources allocated to spiritual care and enhance quality outcomes by improving communication and coordination in the delivery of patient care.
A TRANSITION TO TRANSFORM PATIENT CARE
Health care is evidence-based. Unless professionals in spiritual care and chaplaincy services provide evidence of the benefits of their work, it will go unrecognized. An EMR is a place to record that evidence.
After nearly three years of due diligence, Catholic Health in Buffalo, New York, embarked on an initiative to uniformly manage and implement a new EMR system, using technology provided by Epic, across the organization's five hospitals, ambulatory clinics, home health agencies and other service locations. The primary goals were to create an integrated, standardized EMR platform across its ministries and to use this transition as a catalyst for operational improvement and performance transformation.
All applications launched across the health system on November 1, 2020, creating a unified EMR. The project had six phases, beginning with preplanning activities in February 2019 and ending with post "go-live" optimization, which continues today.
DESIGN: SPIRITUAL CARE ASSESSMENT, INTERVENTION, OUTCOMES TOOL AND WORKFLOW
The first step in the EMR design phase was to meet with the inpatient clinical documentation analyst, the inpatient clinical documentation principal trainer and the interdisciplinary Clinical Decision Support team to evaluate the initial documentation screens and map workflows, defining the care variables by engaging those who would use the system. Doing so also helped to reveal common language across disciplines, ensuring clear communication in the records. Adapting standardized nursing terminology also helped to support and strengthen chaplain/spiritual care documentation and allowed us to better communicate spiritual assessments, interventions and outcomes to nurses and physicians.
For spiritual care providers, the planning process included evaluating the current chaplain reporting needs and workflows; identifying key variables; reviewing system functionality and documentation needs; and picking spiritual care assessments, interventions and outcomes already utilized across the country in the Epic system. Several different documentation models were available in the Epic UserWeb to choose from. The UserWeb is a virtual home where the Epic community can share information, assessment tools and ideas across organizational borders.
During this phase, we had a few objectives. First, we wanted to choose documentation screens used in practice by others with minimal change. Second, we aimed to ensure documentation screens would require minimal time to complete at the point of care (a few minutes per patient). Third, we sought to implement a documentation system that allowed spiritual care providers to enter information relevant to the patient's plan of care and was visible to and easily accessed by all clinical team members. This was important for the spiritual care providers because members of the interdisciplinary team did not easily view their documentation in the previous EMR, often going unnoticed or disregarded. Finally, one of our goals was to develop a dashboard in Epic.
In an environment that embraces an interprofessional, medical-psychosocial and spiritual model of care, a dependable chaplain assessment plan of care with interventions and outcomes is critical. Accurate and consistent assessments and plans of care clearly communicate the spiritual needs of patients/families to the entire health care team and other chaplains who also provide care.
With Epic, Catholic Health had the Spiritual Services Interventions Flowsheet documentation tool created, which includes five screens that identify the reason for the visit, the spiritual assessment of the patient or family, the chaplain intervention(s), the outcome of the visit and the ongoing plan of care.
Once this information is documented by the chaplain, it can then be used by the patient's health care team to assess their spiritual needs, and per the evaluation, the findings that affect health and healing are then incorporated into the care plan. Such an assessment includes data about specific religious beliefs and practices, the role of spirituality and religion in coping with illness, and spiritual and existential suffering caused by illness, accident or the anticipated death of a loved one. Further, the inclusion of the spiritual needs of both patient and family is considered essential to whole-person care1 and is increasingly recognized as a key factor impacting length of stay, aggressive/life-prolonging care and patient/family satisfaction.2
Highlighting the importance of the Spiritual Services Interventions Flowsheet, Catholic Health Chaplain Jonathan Moran says, "I have found flowsheets helpful in capturing the spiritual care assessment. In many ways, the flowsheet format builds on and expands similar concepts chaplains were used to reporting in our previous EMR." Spiritual services are available to all patients — whether they identify as religious, spiritual, both or neither — and are offered without preconceptions or judgment. Healing has always been a vital ministry of the church, and institutional chaplaincy plays a pivotal role in its mission in reaching all community members, including those untouched by the parish.
The EMR can also generate monthly reports that describe the number (percentage of inpatients seen, percentage seen within 24 hours) and type (crisis, routine, sacramental) of chaplain visits, time spent with patients, and type of care provided (pastoral interventions and outcomes). This documentation redesign integrated spiritual information in patient care and provided timely, asynchronous communication between chaplains, nurses and other interdisciplinary team members to promote holistic care. The chaplain enters information into the EMR relevant to the patient's medical, psychosocial and spiritual/religious goals of care. Documentation should only include factual details and should keep information pertinent, clear and informative without violating patient privacy or clergy-congregation relations.3
A chart note enables chaplains to provide the team useful information about the patient that they may not be aware of. For example, a patient may say to the chaplain that his/her spouse died recently and may not have mentioned this significant life event to medical staff during previous treatments. Charting is a way for the rest of the team to see how the spiritual needs and issues of the patient can impact the outcome of their health care experience.
Documentation based on reliable measures contributes to developing evidence-based practice and enhances interprofessional communication and collaboration in achieving desired patient care outcomes. This streamlined communication between chaplains and the clinical care team benefits all patients, including those receiving palliative care and those in critical care units where timeliness is essential to delivering the highest quality of care.
DASHBOARDS AND OUTCOMES
Dashboards and outcomes are analytic tools that allow health care professionals to make real-time, data-driven decisions by compiling information from multiple sources into one view. Dashboards offer insights into organization/department performance compared to benchmarks — and automatically display those metrics in real-time.
Almost all Epic applications have Epic-released dashboards and reports to support workflows and analyze areas for improvement. We reached out to the company and learned that there was no Epic-released dashboards and reports related to spiritual care. With the help of one of this article's authors, Jessica Moore, senior clinical and business intelligence technical analyst, we devised a plan to design a dashboard within Epic itself. The dashboard was largely based on a study previously conducted by Providence Health System in 2000, called Spiritual Needs and Chaplaincy Services: A National Empirical Study on Chaplaincy Encounters in Health Care Settings, with some new metrics added.4
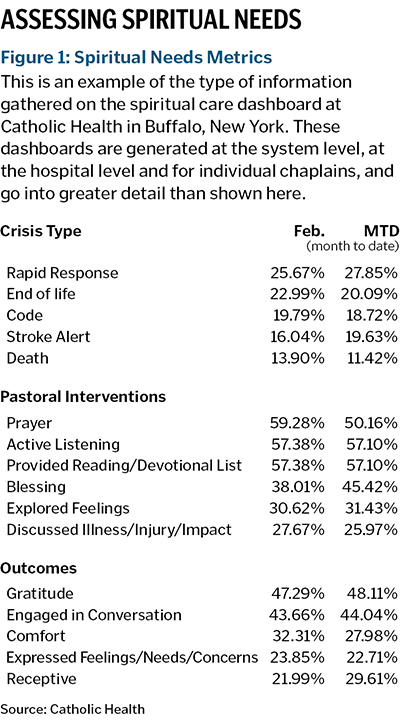
The dashboard is comprised of two sections. (See Figure 1). The left section displays "spiritual needs metrics." The metrics include the type of visit (crisis or routine), the pastoral interventions during the visit and visit outcomes.
A dashboard user can sort the responses by percent, to easily view the top five responses for each category. Data like this enables mission and spiritual care leadership to prioritize patients' values and to customize ongoing education for chaplains.
While prayer, blessings, active listening and providing presence are common, we also see that chaplains discussed an illness/injury and its impact about 27% of the time.
Chaplains have these discussions to help patients, their families and the clinical team when there are questions or disagreements about treatment options and care plans. Furthermore, it is especially significant during end-of-life care planning and palliative care conversations as chaplains help patients identify their hopes and goals related to their current admission.
The dashboards track more than what's shown here, and some of the data relates to other factors.

The right section of the dashboard (see Figure 2) starts with "chaplain performance metrics" and is designed to analyze the performance of our staff chaplains within our hospitals. This gives leadership, including the nursing, mission leader and senior executives, the ability to monitor the percentage of patients seen, the average time spent with patients, usage of different sections of the flowsheets and more. These metrics help identify areas of strength and improvement. For example, our chaplains currently see between 70-80% of inpatients in our hospitals, spending an average of 12 minutes with each patient. Leadership can analyze these numbers against goals for the chaplains and take action as needed.
On a practical level, this data can be used by chaplains in their daily ministry. With the information available from the dashboard shown in Figures 1 and 2, they can more effectively customize their lists and prioritize patients needing to be seen, providing a better experience and improved outcomes for patients. Furthermore, these dashboards provide chaplains the ability to better plan their days. This is especially beneficial on weekends, when there are fewer chaplains in-house. It allows them to triage and prioritize their visits as they respond to numerous codes, rapid responses and deaths.
The data previously described is displayed at an overall system level or by a hospital, and many metrics are available to view for an individual chaplain's performance. The data can be aggregated over days, weeks, months, quarters and years, allowing leadership to monitor trends across various periods of time.
There are also a few detailed reports that are linked on the dashboard, helping leadership understand more specific information about our patients and chaplains. These reports show the progress notes that chaplains are writing; the patients in our hospitals who identify as Catholic, better enabling us to identify those who may like to receive Communion or the sacrament of the Anointing of the Sick; and the patients who have passed away in the last week with their next of kin referenced, helping to assist in sending condolences.
In order to effectively utilize the data gathered on the dashboard, the Spiritual Care departments began receiving weekly electronic reports of chaplain documentation chart notes indexed by, among other fields, individual users. Reports enabled the department to identify key delivery metrics of chaplain productivity and compliance with the scope of service expectations (for example, attendance at every trauma, code and death). They also allowed for the examination of documentation patterns for individual chaplains and clinical pastoral education students, in addition to composite department patterns.
OTHER FINDINGS
Another key component of the weekly report is the tracking of "flowsheet timeliness," which shows the duration of time between the visit and when the chaplain documents it in the patient's chart. Epic thrives on the timely charting of patient encounters so the interdisciplinary team can have a complete snapshot of all caregivers' interactions with the patient. Since all users in Epic can easily find and view a chaplain's documentation, the old practice of waiting until the end of a chaplain's shift to chart is no longer practical.
This information has gone beyond data collection and is now being used to improve daily charting practices for chaplains. Having information to share with the chaplains on ways they could improve the timeliness of charting and flowsheet usage has proven to be extremely valuable. Catholic Health Chaplain Cindy Short says she finds Epic to be a "very helpful tool both in communication for timely follow-up with patients and seamless flow of services, as well as for my own accountability and progress in charting."
An initial review of the reports revealed considerable user variance in spiritual assessment documentation patterns despite similar training at orientation.
These weekly reports serve as more than data collection, allowing for ongoing learning opportunities and professional development. As a pilot program to improve documentation and charting practices at one of our hospitals, the mission leader held one-on-one meetings with chaplains from their team with a specific focus on reviewing the dashboard and weekly Epic reports.
The mission leader and chaplains reviewed the dashboard from a system perspective, the individual hospital perspective and finally from the individual chaplain's viewpoint. In reviewing the weekly reports, the mission leader and chaplain discussed previously mentioned adherence to the scope of service and observed any noticeable trends with the chaplain's charting practices (for example, if they only charted in certain flowsheet rows while overlooking others, and if chaplains were writing progress notes for each of their encounters).
Initially, the chaplains viewed these meetings with a bit of skepticism and anxiety, not knowing if the mission leader would use the weekly reports in a punitive manner. After explaining and demonstrating that the meetings were for individual professional growth and team building to deliver more efficient, patient-centered care, the chaplains embraced the opportunity to review the data. To promote a more consistent system-wide approach, the other mission leaders were encouraged to hold similar meetings with their Spiritual Care and Chaplaincy Services teams once the pilot program was shown to be successful, resulting in improved documentation outcomes.
RECOMMENDATIONS
Spiritual care and chaplaincy services perform a variety of roles in today's complex health care system. Through the EMR, chaplains can demonstrate how valuable the full range of provided psychosocial and spiritual care services are — from assessments, plan of care and outcomes. The daily workflow of chaplains, what they do and the variety of roles performed must be clear. Unclear or confusing roles result in decreased use of spiritual care services, fewer referrals, less participation on committees and diminished credibility within the institution.
The EMR provides a doorway to various scientific methods, such as quantitative and qualitative case studies, scientific baselines and evidence-based data that can springboard further research. A dashboard can serve to stratify patient needs to prioritize follow-up chaplain visits, quantify chaplain visits to determine individual and overall patient needs, and measure the effectiveness of these visits on a patient's spiritual needs.
The professionals in spiritual care and chaplaincy services need to continue to chart and document the visits they make and the services they provide as part of their daily routine. While charting is a requirement by the Joint Commission and other regulating bodies, chaplains are often so caught up with the daily pressures of their job that they tend to neglect to chart, depriving caregivers of good data on which policy decisions can be made.
In an environment of cost-cutting measures, declining reimbursement and high economic pressures, justification for clinical chaplaincy services requires accountability for the services and their effectiveness. Dashboards that clarify what chaplains do, how they do it, how they compare to their peers and that establish baselines and thresholds of performance can not only advance their work but shift to an evidence-based model.
Fulfilling the potential of the evidence-based paradigm would require chaplains to be research literate. They would need to be familiar with the existing body of chaplaincy research, critically read, understand basic research and, if indicated, apply the findings of research studies to one's practice. Correspondingly, the Association of Professional Chaplains does require board certified chaplains (BCC) to do at least five hours of research annually as part of their continuing education.
Therefore, we highly recommend that a concerted effort be made to benchmark some of the services provided by spiritual care departments. Doing a deeper dive into the data can help chaplains be better engaged through a process of dialogue with leadership, administrators, sponsors and the community who can be advocates for an expanded vision of pastoral and spiritual care. Although some chaplain visits (initial and follow-up) are more time-consuming and involve many resources, numerous studies and research shows the correlation between these visits and a better overall patient experience and shorter length of stay.5
Aside from being involved in advance care planning conversations, chaplains also serve as facilitators in resolving conflict and negotiating meaningful goals, especially when patients and families want "everything done" and such requests are medically nonbeneficial. Providing care for patients and families at the end of life, including palliative care, is frequently a priority for spiritual care and chaplaincy services. With the data now available by using a dashboard, spiritual care providers — who may have been previously undervalued by their organization — are now better able to show their worth and impact in the care of patients and families.
NEXT STEPS
In-depth assessments, consultations and counseling services provided by professional chaplains are a necessary part of an integrated and comprehensive biopsychosocial-spiritual approach to assessing a patient's needs, preferences and goals of care. An EMR can inform evidence-based practice, and research elsewhere has shown that the services provided by professionals in spiritual care and chaplaincy services are measurable and provide significant benefits.
One direction for ministries moving forward might be developing spiritual care services as a reimbursable service, like other aspects of health care. An attempt must be made to explore a case for reimbursement from payers and insurers for services provided. For example, hospices are required to provide an assessment of the patient and their family's spiritual needs, provide counseling to address them and make reasonable efforts to facilitate visits by local clergy, pastoral counselors or other qualified individuals. In hospice, the chaplain is the only member of the interdisciplinary team who cannot report visits on the claim form, and this needs to change. An EMR can communicate the value of spiritual care to patients and payers.
Chaplains have entered a paradigm in which they can demonstrate how integral they are to an interdisciplinary team of health care professionals providing services to patients, long-term care residents and their families. An EMR can provide sufficient empirical clinical evidence to support spiritual care as a legitimate and positive component of the patient's holistic treatment plan. The moment has come to ask: What kind of future can chaplains look forward to?
The future depends, as it always has, on how much chaplains are willing to critically review the assumptions, models and structures under which they operate. The road ahead for chaplaincy will largely depend on the quality of both charting and the data entered in an EMR. Properly utilized, dashboards can provide greater accountability, requiring chaplains to be more intentional in their practice and focused on outcomes than they have been in the past. The extent to which chaplains utilize intentional, outcome-focused or evidence-based practices and dashboards will largely determine the degree to which spiritual care is established, maintained and integrated into the total interdisciplinary health care continuum.
Budgets for clinical professional chaplaincy services need to be based on value, sponsorship and the reputation of the mission and identity of an institution. While Catholic health care ministries focus on the quality of our pastoral care services and hold this work in high esteem, reputation alone isn't enough. Clinical professional chaplaincy services need to be based on value and measurable ways to track that value. Having good empirical data can only strengthen the need for clinical professional chaplaincy services during a time of continued economic challenges. Through the proper use of data-driven tools and resources, the future role of professional clinical chaplains in health care can be elevated beyond an ornament of mission and identity, and instead as an integral part in the transformation of patients' health and healing.
BARTHOLOMEW RODRIGUES is executive vice president and chief mission officer for Catholic Health, Buffalo, New York. WILLIAM VAUGHAN is vice president of mission integration for Mercy Hospital of Buffalo, Buffalo, New York. JESSICA MOORE is senior clinical and business intelligence technical analyst, information technology, Catholic Health, Buffalo, New York.
NOTES
- Judy E. Davidson et al., "Clinical Practice Guidelines for Support of the Family in the Patient-Centered Intensive Care Unit: American College of Critical Care Medicine Task Force 2004–2005," Critical Care Medicine 35, no. 2 (February 2007): 605-22, https://doi.org/10.1097/01.CCM.0000254067.14607.EB.
- Tracy Anne Balboni et al., "Provision of Spiritual Care to Patients With Advanced Cancer: Associations With Medical Care and Quality of Life Near Death," Journal of Clinical Oncology 28, no. 3 (January 2010): 445-52, https://doi.org/doi:10.1200/jco.2009.24.8005.
- Rabbi Stephen B. Roberts, Professional Spiritual & Pastoral Care: A Practical Clergy and Chaplain's Handbook (Nashville: SkyLight Paths Publishing, 2011): 81-91.
- Bartholomew Rodrigues, Deanna Rodrigues, and D. Lynn Casey, Spiritual Needs and Chaplaincy Services: A National Empirical Study on Chaplaincy Encounters in Health Care Settings (Medford, Oregon: Providence Health System, 2000).
- Paul Alexander Clark, Maxwell Drain, and Mary P. Malone, "Addressing Patients' Emotional and Spiritual Needs," Joint Commission Journal on Quality and Patient Safety 29, no. 12 (December 2003): 659-70, https://doi.org/10.1016/s1549-3741(03)29078-x.